Knee Problems: Meniscal injury
KNEE PROBLEMS
SURGICAL PROCEDURES
Meniscal Function
The meniscus is important for transmitting loads across the knee. The menisci increase the surface area of contact and fill the gaps between differently shaped articulating surfaces: the round femoral condyles, the relatively flat tibial plateau on the medial side, and the convex tibial plateau on the lateral side.
 |
|
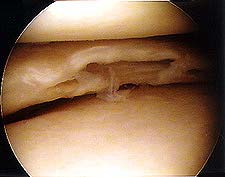
| Normal medial meniscus |
Removing the menisci increases the contact pressure between the femur and the tibial articular surfaces and may predispose to early arthritis. On the medial side, load is shared equally between the medial meniscus and the articular surface. However, the lateral meniscus must bear most of the lateral side load transmission alone. It seems that degenerative changes are more likely after partial lateral meniscectomies than after partial medial meniscectomies.
The meniscus has been shown to play a vital role in load transmission across the knee joint. Biomechanical studies have demonstrated that at least 50% of the compressive load of the knee joint is transmitted through the meniscus in extension, and 85% of the load is transmitted in 90 degrees of flexion. In the meniscal deficient knee the contact area is reduced approximately 50%, which results in articular cartilage damage. Partial meniscectomy has also been shown to increase contact pressures significantly. Another proposed function of the meniscus is that of schock absorption, although it seems that the menisci do not play a significant role in shock absorption. The menisci are also believed to contribute to joint stability, especially in ACL deficient knees. Finally, the menisci may serve as proprioceptive structures providing a feedback mechanism for joint position sense.
Meniscal Injury
Turning or twisting of the knee may cause tearing of the meniscus. When the torn part is mobile, flexion and extension of the knee can displace the fragment out its normal position. Typical signs and symptoms are clicking, catching or snapping. A knee effusion may or may not be present, but most patients will have jointline tenderness.
 |
 |
|
Radial meniscal tear |
Large meniscal flap tear |
Giving way and locking are also frequent symptoms of a meniscal injury. Displaced bucket handle tears, which usually go with chronic ACL deficiency, will cause the knee to lock in flexion. Anteromedial pain with mechanical block to extension reflects a displaced bucket-handle tear or ACL tear.
 |
 |
|
Longitudinal tear |
Bucket handle tear |
Medial meniscal tears are more often symptomatic than lateral meniscal tears. Most tears occur in the posterior load-bearing area, causing medial and posteromedial jointline pain and effusion. Pain in the anterior third is not from a meniscal tear, because no weightbearing occurs there, and anterior medial meniscal tears are extremely rare. However, patients with a displaced bucket-handle medial meniscal tear may complain of anteromedial pain with a mechanical block to extension, which is often followed by an effusion.
Early clinical and MRI diagnosis, and appropriate treatment of meniscal tears, especially in people younger than 40, are very important for the longevity of the knee joint.
Meniscal Cysts
Meniscal cysts were first described by Ebner in 1904. They are often associated with a specific complex type of meniscal tear called a horizontal cleavage tear, usually of the lateral, rarely the medial meniscus. However, isolated cysts without meniscal pathology have also been reported. Clinically, meniscal cysts look like a small lump, usually at the level of the lateral joint line. The size of the lump often correlates to activity level and the chronicity and the complexity of the meniscal tear. They are encapsulated, hernia-like structures, and they contain viscous synovial, often gel-like, fluid which penetrates through the torn meniscus and accumulates under the skin.
Several theories have been proposed regarding cyst aetiology, including traumatic and degenerative origins. Histology shows a meniscal cyst formation which originates by influx of synovial fluid through microscopic and gross tears in the substance of the meniscus. A meniscal tear with a horizontal component, as well as a tract that provides an exchange of fluid between the joint and the cyst, is often seen. Meniscal cysts are multilocular and lined with synovial endothelial tissue.
Meniscal cysts can be drained with a needle (although this can be difficult because of the viscosity of the content of the cyst) but they will often come back, because a tear in the meniscus will allow further penetration of the synovial fluid into the cyst. The management of a meniscal cyst usually involves an MRI scan of the knee to determine the presence of a meniscal tear and the location of the cyst. In the presence of a meniscal tear, partial arthroscopic meniscectomy followed by arthroscopic cyst decompression is the treatment of choice. If a tear is not confirmed at the time of arthroscopy open decompression of the cyst, performed through a mini-arthrotomy, combined with "outside-in" meniscal repair is the best treatment option. Recurrent meniscal cysts are not uncommon and open cystectomy may be required. In any case, the peripheral meniscal body should be preserved and the meniscus should not be excised under any circumstances.
|
 Lateral meniscal cyst |
Clinically lateral meniscal cysts are far more common than the medial ones. However, MR imaging reveals a different pattern. A retrospective review of 2572 knee MRI reports, for the presence of meniscal tears and cysts, revealed that meniscal cysts occur almost twice as often in the medial compartment as in the lateral compartment! Medial and lateral tears occur with the same frequency. These findings, when viewed in the context of the historical literature on meniscal cysts, suggest that MR imaging detects a greater number of medial meniscal cysts than physical examination or arthroscopy, and that MR imaging can have an important impact on surgical treatment of patients.
- Source: Campbell SE at al.: MR Imaging of Meniscal Cysts - Incidence, Location and Clinical Significance. American Journal of Roentgenology 2001; 177: 409 - 413.
Further Information:
- Yu WD, Shapiro MS. Cysts and Other Masses About the Knee: Identifying and Treating Common and Rare Lesions. The Physician and Sportsmedicine, July 1999. Please note that free access to this article is no longer available.
Discoid Meniscus
A discoid meniscus is a congenital anatomical variant that involves the lateral meniscus significantly more than the medial meniscus. The incidence of this variant in several clinical studies ranges from 0.4% to 17%, while the incidence in a large cadaver study was 5%. The most common symptoms of discoid meniscus, which usually occur during childhood and adolescence, are pain, locking, and a snapping or a clunking sound. These symptoms can occur with both intact and torn discoid menisci. However, symptoms are most frequently a result of a peripheral tear of the central discoid portion of the meniscus. MRI is the modality of choice to evaluate a discoid meniscus before surgery. The traditional treatment for mechanically symptomatic torn discoid meniscus has been a partial arthroscopic meniscectomy, but more recently several authors have reported results of surgical repair. Extensive subtotal or total lateral meniscectomy of the discoid meniscus is best avoided.
Further Information:
- Ralph Di Libero, MD. Discoid Meniscus. eMedicine article, last updated: October 18, 2006.
Partial Meniscectomy
If you have a meniscal tear (typically a displaceable flap tear of either meniscus) which is causing you mechanical problems (clicking, catching, locking) careful arthroscopic partial meniscectomy is often the quickest way to solve this problem and restore knee function. Losing a small, already torn, part of the meniscus is not a major problem in the long run, providing that the knee is stable and that articulating surfaces are not worn out. However, complex meniscal tears are often associated with unstable ligaments and damaged articular surfaces, and surgical removal of most of the meniscal tissue is associated with acceleratd wear and tear.
Further information:
- 3D Animation: Torn Meniscus Trimming. Understand.com in partnership with AOSSM.
- I. D. McDermott and A. A. Amis: The consequences of meniscectomy. Journal of Bone and Joint Surgery - British Volume, Vol 88-B, Issue 12, 1549-1556 (2006).
- K. Donald Shelbourne and Jonathan F. Dickens: Digital Radiographic Evaluation of Medial Joint Space Narrowing After Partial Meniscectomy of Bucket-Handle Medial Meniscus Tears in Anterior Cruciate Ligament–Intact Knees.
The American Journal of Sports Medicine 34:1648-1655 (2006).
Meniscal Repair
Most meniscal injuries do not require treatment apart from displaceable tears which are causing recurrent mechanical problems, including locking. In young people, if diagnosed early and before the structural damage occurs, meniscal tears in the vascular zone can be repaired very successfully arthroscopically. Early MRI diagnosis and appropriate meniscal repair, rather than partial meniscectomy, are very important. However, in our experience, most meniscal tears are not repairable, either because the meniscus is already structurally damaged, or the tear is in the avascular zone. The functional outcomes of meniscal repair in this group are not very good.
 |
 |
|
| Displaced bucket-handle meniscal tear |
Repairable meniscal tear in the vascular zone |
Meniscal Implants
Menaflex™ collagen meniscus implant (formerly CMI®) is a device designed to guide new tissue growth using the body’s own healing process in patients with an irreparable meniscus tear or loss of meniscus tissue. It provides a resorbable scaffold for the growth of new tissue in the meniscus. There are Menaflex devices designed specifically for use in the lateral meniscus and medial meniscus. This is a new meniscal implant in the UK. Only a few have been implanted so far (November 2008) and early functional outcomes are not yet available.
Further information:
- William G. Rodkey, et al.: Comparison of the Collagen Meniscus Implant with Partial Meniscectomy. A Prospective Randomized Trial.
The Journal of Bone and Joint Surgery (American). 2008;90:1413-1426.
New Meniscal Repair Device
Meniscal tears are difficult to repair successfully. Most of the adult meniscus is avascular, meaning that it does not have a good blood supply and therefore does not heal well. Because two-thirds of the meniscus is avascular, a tear in that region will not repair itself. Surgeons call this portion of the meniscus the "white zone." The "red zone" of the meniscus is well vascularized tissue which can be repaired in certain situations. However, the new meniscal repair device, called the BioDuct, will transport blood and cells from the vascular portion of the knee to the avascular portion of the meniscus. Supplied with blood and cells for healing, the previously untreatable meniscal tear now has the potential to heal and protect the joint over a sustained period of time. Currently, there is no other device on the market that can provide improved fixation over time. The use of BioDuct has been approved by the FDA for human use. For more information click on University of Missouri News Bureau Press Release. This exciting new product was developed by Schwartz Biomedical LLC and it will be marketed internationally by Stryker Corporation. Mr Bobic participated in designing the clinical concept and the surgical technique with a number of US researchers and clinicians, as a member of the clinical advisory board. This device is not yet available in the UK.
Further information:
- James L. Cook and Derek B. Fox, from the Comparative Orthopaedic Laboratory, University of Missouri, Columbia, Missouri, USA, published an article A Novel Bioabsorbable Conduit Augments Healing of Avascular Meniscal Tears in a Dog Model in the November 2007 issue of the American Journal of Sports Medicine. They conclude: "conduit treatment resulted in functional healing with bridging tissue and biomechanical integrity in 71% of avascular meniscal defects for up to 6 months after surgery. No functional healing was noted in avascular meniscal tears treated by trephination and suture repair."
Further information on meniscal injuries and repair:
- Sarjoo M Bhagia, et al.: Meniscal Injury. eMedicine article, last updated August 30, 2006.
- For further information on meniscal injuries please visit Steadman-Hawkins Clinic website.
- Gregory P. Lee and David R. Diduch: Deteriorating Outcomes After Meniscal Repair Using the Meniscus Arrow in Knees Undergoing Concurrent Anterior Cruciate Ligament Reconstruction. Increased Failure Rate With Long-term Follow-up. The American Journal of Sports Medicine 33:1138-1141 (2005).
- Gabriela von Lewinski, et al.: The Influence of Nonanatomical Insertion and Incongruence of Meniscal Transplants on the Articular Cartilage in an Ovine Model. The American Journal of Sports Medicine 36:841-850 (2008).
Page last updated on: 13 May 2018
Site last updated on: 28 March 2014
|
[ back to top ]
 Disclaimer: This website is a source of information
and education resource for health professionals and individuals
with knee problems. Neither Chester Knee Clinic nor Vladimir Bobic
make any warranties or guarantees that the information contained
herein is accurate or complete, and are not responsible for
any errors or omissions therein, or for the results obtained from
the use of such information. Users of this information are encouraged
to confirm the accuracy and applicability thereof with other sources.
Not all knee conditions and treatment modalities are described
on this website. The opinions and methods of diagnosis and treatment
change inevitably and rapidly as new information becomes available,
and therefore the information in this website does not necessarily
represent the most current thoughts or methods. The content of
this website is provided for information only and is not intended
to be used for diagnosis or treatment or as a substitute for consultation
with your own doctor or a specialist. Email
addresses supplied are provided for basic enquiries and should
not be used for urgent or emergency requests, treatment of any
knee injuries or conditions or to transmit confidential or medical
information. If you have sustained a knee injury or have a medical condition,
you should promptly seek appropriate medical advice from your local
doctor. Any opinions or information,
unless otherwise stated, are those of Vladimir Bobic, and in no
way claim to represent the views of any other medical professionals
or institutions, including Nuffield Health and Spire Hospitals. Chester
Knee Clinic will not be liable for any direct, indirect,
consequential, special, exemplary, or other damages, loss or injury
to persons which may occur by the user's reliance on any statements,
information or advice contained in this website. Chester Knee Clinic is
not responsible for the content of external websites.
Disclaimer: This website is a source of information
and education resource for health professionals and individuals
with knee problems. Neither Chester Knee Clinic nor Vladimir Bobic
make any warranties or guarantees that the information contained
herein is accurate or complete, and are not responsible for
any errors or omissions therein, or for the results obtained from
the use of such information. Users of this information are encouraged
to confirm the accuracy and applicability thereof with other sources.
Not all knee conditions and treatment modalities are described
on this website. The opinions and methods of diagnosis and treatment
change inevitably and rapidly as new information becomes available,
and therefore the information in this website does not necessarily
represent the most current thoughts or methods. The content of
this website is provided for information only and is not intended
to be used for diagnosis or treatment or as a substitute for consultation
with your own doctor or a specialist. Email
addresses supplied are provided for basic enquiries and should
not be used for urgent or emergency requests, treatment of any
knee injuries or conditions or to transmit confidential or medical
information. If you have sustained a knee injury or have a medical condition,
you should promptly seek appropriate medical advice from your local
doctor. Any opinions or information,
unless otherwise stated, are those of Vladimir Bobic, and in no
way claim to represent the views of any other medical professionals
or institutions, including Nuffield Health and Spire Hospitals. Chester
Knee Clinic will not be liable for any direct, indirect,
consequential, special, exemplary, or other damages, loss or injury
to persons which may occur by the user's reliance on any statements,
information or advice contained in this website. Chester Knee Clinic is
not responsible for the content of external websites.