Rehabilitation
SEE ALSO
Introduction
Rehabilitation is the key to successful functional recovery after knee injuries and surgery. Early motion and weightbearing are essential for successful rehabilitation outcomes. The Physiotherapist must understand the anatomy and the biomechanics of the knee joint, the pathophysiology of the particular injury, the principles of the particular surgical procedure, and the process of tissue healing. Equally, the surgeon should provide detailed perioperative information, and discuss any special requirements with the physiotherapist. The three-way communication (surgeon-patient-physiotherapist) is very important for the progress and the outcome of postoperative knee rehabilitation.
Phases of Knee Rehabilitation
Individual rehabilitation programme following knee injury or surgery should be developed on the basis of the knee structures injured, the severity of the injury, the surgical procedure, and the goals of the patient and the physiotherapist. Rehabilitation programs should follow a protocol of ongoing pain and swelling control to aid in establishing and maintaining early range of motion and progressive weightbearing. Each phase of rehabilitation may involve the performance of isometrics, isotonics, isokinetics, balance and proprioception, endurance, power, and functional or sport-specific activities.
 |
The Aircast® Cryo/Cuff combines focal compression with cold to provide optimal control of swelling, oedema, haematoma, hemarthrosis, and pain. | ||
Phase 1 involves posttraumatic or postsurgical management of swelling, pain, inflammation and joint dysfunction. This phase may involve joint protection by immobilisation, bracing, and limited weightbearing until the patient can walk without a limp. Inflammation occurs to the knee joint in both injury and after surgery. Managing the inflammatory response after knee injury or surgery includes controlling pain and swelling and regulating motion both in the initial phase and throughout the entire rehabilitation process. Ice, elevation, compression, and other treatment modalities are used to manage pain and swelling. Wound management after injury or surgery should be closely monitored. Any signs of an infection should be reported to the surgeon directly.
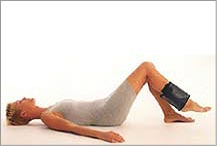
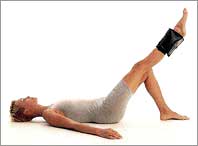
Phase 2 re-establishes full ROM and joint mobility. Strengthening progresses
within tissue-healing constraints. Weightbearing advances according
to strength and level of healing. Endurance exercises are used to maintain
or re-establish fitness. Proprioception and balance advance from low-level,
stable surface training to high-level, unstable-surface training. Light
functional activities can begin at this stage.
 |
 |
Phase 3 continues with advanced progressive resistive exercise, functional activities, and implements speed and power training. Plyometrics (exercises that enable muscles to reach maximum strength in as short time as possible - typically jump training), dynamic balance and proprioception, agility and sport-specific training are intensified, protections and limitations gradually decrease during this phase.
Phase 4 involves return-to-play criteria. Simulated competition and skill
refinement are important to return to play in a competitive environment.
The ability to return to play should be based on satisfactory performance
on various tests, including an isokinetic evaluation, negative clinical
examination, functional tests and psychological state of readiness.
|
Proprioceptive Exercises
These are exercises that help retrain your position sense, also called
"joint sense". If you close your eyes and bend your knee,
you know what your knee is doing, even though you don't "see"
it. This ability enables us to know where our limbs are in space without
having to look. It is important in all everyday movements but especially
so in complicated sporting movements, where precise coordination is
essential. This coordinated movement is a result of the normal functioning
of the proprioceptive system. We get position sense by way of our vision,
middle ear balance, and from tiny receptors in the ligaments and joints.
When we close our eyes, we rely on middle ear balance and these special
receptors to keep us upright. The proprioceptive system is made up of
receptor nerves that are positioned in the muscles, joints and ligaments
around joints. The receptors can sense tension and stretch and pass
this information to the brain where it is processed. The brain then
responds by signalling to muscles to contract or relax in order to produce
the desired movement. This system is subconscious, and we don't have
to think about the movements or the corrections to movement. Sometimes
the reactions take place so fast they are termed reflexive.
Following injury to joints and ligaments the receptors are also damaged,
which means the information that is usually sent to the brain is impaired.
As a consequence the joint feels odd or just doesn't feel right. You
can do certain exercises to get the other receptors to do more, regaining
what was lost with the damaged receptors. The loss of position sense
puts the joint at further risk of injury because the loss of stability.
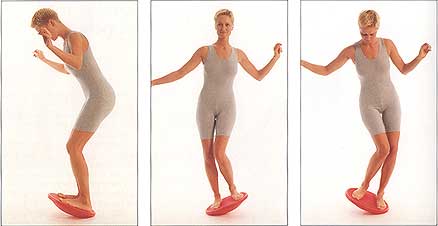
Special exercises, called proprioceptive or neuromuscular exercises,
help protect the knee. You can think of these exercises like balance
training. Examples include balancing on one leg with your eyes open/closed,
walking on uneven or soft surfaces, or practicing on a special balance
board. As early as you can comfortably bear weight through the affected
knee, proprioceptive exercises should be initiated. These improve the
stimuli within the body relating to position and movement. Use wobble
board exercises to improve proprioception. You should balance on the
affected leg for 1 minute, then rest. This can be repeated several times.
Some therapists use special manual exercises to get the other receptors
working better.
| Exercise images reproduced
with permission of Allan Larsen, MD, PhD, Specialist Orthopaedic
Surgeon, Aalborg, Denmark. Source: All Round Fitness, Centrum A/S, Denmark 1995. Images: Poul Ib Henriksen. |
|
 |
Further information:
- Raphael Brandon: Proprioception: balance, stability and Swiss ball exercises. Sports Injury Bulettin.
- Owen Anderson: Proprioceptive exercises training programme. Sports Injury Bulettin.
- Edward R. Laskowski et al.: Refining Rehabilitation With Proprioception Training: Expediting Return to Play. The Physician and Sportsmedicine, October 1997. Please note that free access to this article is no longer available.
Plyometric Exercises
Plyometric exercising refers to exercise that enables a muscle to reach maximum force in the shortest possible time. The muscle is loaded with an eccentric (lengthening) action, followed immediately by a concentric (shortening) action. Plyometrics is one of the best ways to develop sport-specific power. But you must have a well-designed program structure for them to be truely effective. Further information: Sport Fitness Advisor
Gait Analysis
Most commonly, observational gait analysis is appropriate to characterize most gait pathologies. This approach is sufficient to note gross abnormalities in walking; however, as walking complexity increases with organic pathology, objective analysis becomes necessary. The measurement systems that follow may be used individually or collectively. The choice of method is based on clinical need, financial considerations, and staffing at the specific laboratory. Typically, motion and force data are compiled simultaneously. Further information:
- Ross Bogey, DO. Gait Analysis. eMedicine article. Last updated February 21, 2007.
Cycling for Knee Rehabilitation
Exercise bikes, static bikes, stationary cycles, bicycle ergometers - these are all names for the bicycles that you find in virtually every physiotherapy clinic, gym or health club across the world. Many knee rehabilitation protocols include cycling so why is this exercise modality so popular for knee rehabilitation? In comparison with other exercises cycling is a relatively ?knee friendly? activity that can help to improve knee joint mobility and stability. Cycling is frequently used as a rehabilitation exercise modality after knee injury or surgery as well as part of the management of chronic degenerative conditions such as osteoarthritis. This article will give you an insight into the use of a cycle for knee rehabilitation:
- Karen Hambly: Cycling for Knee Rehabilitation. Cartilage Health 2009.
- For specialist bicycle adaptations see Chris Bell's website: Highpath Engineering Specialist Services.
"Footnotes" on Knee Pain
Many of knee problems are created or compounded by the knee being subjected to transverse plane motion generated by internal or external tibial rotation secondary to the foot's excessive pronation or supination. On this basis, stabilisation of the foot will often lead to a reduction in the knee symptoms by reducing both the magnitude and velocity of transverse plane motion within the last 15 degrees of motion that precedes full knee extension. Shoe inserts, insoles and orthotics can correct a variety of foot biomechanical problems including pronation and supination while they increase stability and provide heel cushioning. For more information please visit Superfeet website.
Further information:
- Thomas D. Rizzo, Jr, MD: Using RICE for Injury Relief. The Physician and Sportsmedicine, October 1996. Please note that free access to this article is no longer available.
- Kris Jensen, MS, PT, SCS: At-home Knee Rehabilitation: Strengthening Without Special Equipment. The Physician and Sportsmedicine, May 1996. Please note that free access to this article is no longer available.
Information on knee braces and supports:
See also:
- For post-operative Procedure-specific Rehabilitation program see our Knee Problems page.
- For an update on Peri-oprative ACL Rehabilitation please see our separate
page on Accelerated ACL Reconstruction
Rehabilitation Program which was kindly written and put together
by Mark De Carlo and his team at the Methodist Sports Medicine Center,
Indianapolis, Indiana, USA.
This page was updated on 12 May 2018
Site last updated on: 28 March 2014
|
[ back to top ]

 Disclaimer: This website is a source of information
and education resource for health professionals and individuals
with knee problems. Neither Chester Knee Clinic nor Vladimir Bobic
make any warranties or guarantees that the information contained
herein is accurate or complete, and are not responsible for
any errors or omissions therein, or for the results obtained from
the use of such information. Users of this information are encouraged
to confirm the accuracy and applicability thereof with other sources.
Not all knee conditions and treatment modalities are described
on this website. The opinions and methods of diagnosis and treatment
change inevitably and rapidly as new information becomes available,
and therefore the information in this website does not necessarily
represent the most current thoughts or methods. The content of
this website is provided for information only and is not intended
to be used for diagnosis or treatment or as a substitute for consultation
with your own doctor or a specialist. Email
addresses supplied are provided for basic enquiries and should
not be used for urgent or emergency requests, treatment of any
knee injuries or conditions or to transmit confidential or medical
information. If you have sustained a knee injury or have a medical condition,
you should promptly seek appropriate medical advice from your local
doctor. Any opinions or information,
unless otherwise stated, are those of Vladimir Bobic, and in no
way claim to represent the views of any other medical professionals
or institutions, including Nuffield Health and Spire Hospitals. Chester
Knee Clinic will not be liable for any direct, indirect,
consequential, special, exemplary, or other damages, loss or injury
to persons which may occur by the user's reliance on any statements,
information or advice contained in this website. Chester Knee Clinic is
not responsible for the content of external websites.
Disclaimer: This website is a source of information
and education resource for health professionals and individuals
with knee problems. Neither Chester Knee Clinic nor Vladimir Bobic
make any warranties or guarantees that the information contained
herein is accurate or complete, and are not responsible for
any errors or omissions therein, or for the results obtained from
the use of such information. Users of this information are encouraged
to confirm the accuracy and applicability thereof with other sources.
Not all knee conditions and treatment modalities are described
on this website. The opinions and methods of diagnosis and treatment
change inevitably and rapidly as new information becomes available,
and therefore the information in this website does not necessarily
represent the most current thoughts or methods. The content of
this website is provided for information only and is not intended
to be used for diagnosis or treatment or as a substitute for consultation
with your own doctor or a specialist. Email
addresses supplied are provided for basic enquiries and should
not be used for urgent or emergency requests, treatment of any
knee injuries or conditions or to transmit confidential or medical
information. If you have sustained a knee injury or have a medical condition,
you should promptly seek appropriate medical advice from your local
doctor. Any opinions or information,
unless otherwise stated, are those of Vladimir Bobic, and in no
way claim to represent the views of any other medical professionals
or institutions, including Nuffield Health and Spire Hospitals. Chester
Knee Clinic will not be liable for any direct, indirect,
consequential, special, exemplary, or other damages, loss or injury
to persons which may occur by the user's reliance on any statements,
information or advice contained in this website. Chester Knee Clinic is
not responsible for the content of external websites.