Chester Knee Clinic News 2015
CKC Clinical and Research News
Updated on 29 March 2015
Adipose Tissue Derived Autologous Stem Cells
Since January 2015 we have Chester Nuffield's MAC approval for surgical use of Adipose tissue Stromal Vascular Fraction (Adipose SVF). There is a worldwide consensus that regenerative cells from differentiated autologous body tissues are the most ethical option in regenerative medicine. The general preference for Adipose SVF is based on easy clinical harvest of adipose cells and a huge regenerative cell density (10 to 100 fold more stem cells than other body tissues). We are planning to use this technology as an addition to several standard orthopaedic procedures like autologous osteochondral grafting, subchondral decompression, osteochondral repair and similar. We are comparing different technologies and preparing technical side of introducing this technology to our clinical practice in the summer of 2015.
Lamina Splendens Research
The uppermost layer of hyaline articular cartilage is called Lamina Splendens. This film-like layer is seldom seen arthroscopically and various optical and electron microscopic imaging studies have shown conflicting morphology and structure. Considering its location there is no doubt that Lamina Splendens has extremely important articular function as it provides a very low friction lubrication surface and contains collagen fibrils which run parallel to the surface of articulation. This surface zone layer is likely to play a key role in maintaining the mechanical response of articular cartilage to load. It is the first region of cartilage to degrade in ostroarthritis and yet there is no evidence that it is regenerated when articular cartilage is repaired, not even with autologous chondrocytes. This is a significant limitation that, unless resolved, may lead to the ultimate failure of any articular cartilage implant as a result of the shear forces in the joint. For this reason, it is critical to understand the role of the surface zone of cartilage in development, joint function, and pathology.
As the structure and function of this elusive articular layer remains unclear, we have started collaborative imaging project on morphologic and structural imaging and functional research of animal and human lamina splendens at the Institute of Integrative Biology at the University of Liverpool, UK (Prof Anthony Hollander) and Osaka Health Science University, Japan (Prof Norimasa Nakamura). We will present this project and our preliminary findings at 12th ICRS Congress in Chicago in May 2015.
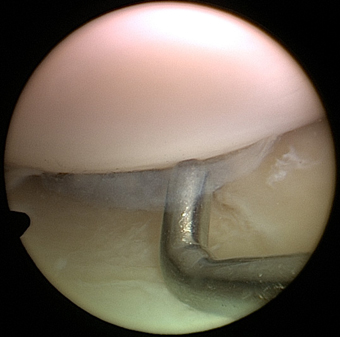
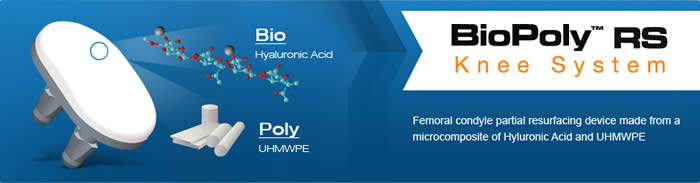
BioPoly™ RS Partial Resurfacing Knee Implant Clinical Trial
We continue to recruit patients for this clinical trial based in Chester (please see a list of Inclusion and Exclusion Criteria). The BioPoly™ first implantation was done early in January 2012 by Mr Dinesh Nathwani at the London Clinic (for more information please see the article from The Telegraph and the article from Mail Online). The first large BioPoly (the "racetrack", picture above) was implanted in April 2012 by Mr Mike McNicholas, at the Warrington Hospital. So far we have implanted 22 BioPoly implants, with good short to mid term functional results.
BioPoly Partal Resurfacing Implant is indicated for patients who present with a painful articular cartilage lesion of the femoral condyle and who is not a candidate for biological treatment (articular cartilage repair) or total joint replacement
Please be aware that we can not enter any potential candidates into the BioPoly clinical trial before they have been seen and examined in person at one of the sites by one of the investigators listed below. Email and telephone communications, however specific or detailed, are not sufficient for the assessment of suitability for this clinical trial.
Although the manufacturer of BioPoly implants will provide all implants free of charge for the duration of the clinical trial, your medical insurer or you will be responsible for all other costs (clinic appointments, imaging such as X-ray or MRI, the costs of the surgical procedure and hospital charges as well as perioperative physiotherapy). This does not apply if you enter the BioPoly clinical trial as an NHS patient (this option is available at Aintree Hospital Liverpool, the Imperial College London and RNOH Stanmore).
BioPoly® Announces 100th Knee Surgery (14 April 2015): Herb Schwartz PhD, President of BioPoly, stated “We are very excited to reach this important milestone. With the longest term patients beyond the 3 year time point, the implants are performing remarkably. Patients can bear weight immediately after surgery and return to normal activities within weeks. They are reporting that they are pain free and are showing marked improvements in their quality of life.”
Participating Centres (in alphabetical order):
- Aintree Hospital, Liverpool, contact: Mr Michael McNicholas, mike.mcnicholas@aintree.nhs.uk
- Chester Knee Clinic at Chester Nuffield, contact: Mr Vladimir Bobic (principal investigator), office@kneeclinic.info
- Royal National Orthopaedic Hospital, Stanmore, contact: Iva Hauptmannova, iva.hauptmannova@rnoh.nhs.uk
- The London Clinic, contact: Mr Dinesh Nathwani, d.nathwani@precisionsurgery.co.uk
Further Information:
- BioPoly general information: www.biolpolyortho.com
- BioPoly Newsletter.
- BioPoly video: http://youtu.be/MbzBSUz_82A
- Clinical Trials (a service of the US NIH): ClinicalTrials.gov (clinical trial identifier: NCT01473199)
- UKCTG - UK Clinical Trials Gateway (NHS National Institute for Health Research): BioPoly Registry Study
CKC Meetings and Conferences
Updated on 5 March 2015
2nd ICRS Summit "The Ageing Cartilage", Zermatt, Switzerland, 15-16 January 2015
Prof Bobic, invited speaker, gave a talk on injured and ageing subchondral bone.
HTA Site Inspection, 12 March 2015, Chester, UK
Scheduled HTA inspection (re procurement HTA licence for ACI surgery) at Nuffield Health, The Grosvenor Hospital Chester
Lamina Splendens Imaging and Research Meeting, 20 March 2015, Liverpool, UK
Initial meeting with Prof Anthony Hollander and his imaging team at the Institute of Integrative Biology, the University of Liverpool.
12th ICRS World Congress, Chicago, USA, 8-11 May 2015
Prof Bobic, invited speaker and moderator presented a first lecture on structure and function of Lamina Splendens "What is Lamina Splendens and What Does It Do?"
Nuffield Health Edicational Seminars, GP Symposium, St. David's Park Hotel, Ewloe, Wales, 24 October 2015
Prof Bobic is giving a talk on Biologics and Stem Cells in Sports Medicine and Orthopaedics
For more information on this topic please see the following links: Biologics for Sports Medicine and Orthopaedic Healing, Sports Medicine Update September/October http://www.sportsmed.org/apps/SportsMedicineUpdate/index.html#p=4
Stem Cells in Orthopaedics, Dr Rohit Vikas
Sports Knee Surgery 2015, St George's Park, near Burton Upon Trent, 2 and 3 November 2015
Prof Bobic will co-moderate a session on Articular Cartilage with Tim Spalding on 3rd November
Recent CKC Orthopaedic and Sport Injury News
Updated on 5 April 2015
ACI: NICE to block use of proven knee articular cartilage repair technology
"NICE has opened a public consultation on its draft guidance on ACI surgery." 12 March 2015
“The independent Appraisal Committee considered the evidence available on ACI (Autologous Chondrocyte Implantation), which included evidence on the nature of knee cartilage damage, the views of people with the condition, those who represent them, and clinical experts. ACI is a promising technology, but there is insufficient long-term evidence to support a conclusion on the long-term effectiveness of its use. This lack of evidence meant that the Committee could not recommend ACI for routine use of NHS resources, but it wanted to encourage further research to generate more evidence on the effectiveness of the procedures considered. Therefore in this draft guidance, the committee recommends that ACI is used in the context of research which should include clinical trials and observational studies designed to measure its long-term benefits. We welcome comments on this draft recommendation as part of the consultation.”
However, this view is not supported by most UK orthopaedic surgeons who specialise in articular cartilage repair and use ACI technology in their practice. The BASK has issued the following statement to its members on 25 March 2015: "As discussed at the BASK Annual Spring Meeting last week, NICE has made an inappropriate provisional judgement on ACI that would deny us options for treating patients using therapies proven to work. The NICE judgement is for NHS patients, but insurers have stated they will not allow ACI either if it is termed experimental. Their provisional decision was based on insufficient review of the literature, misinterpretation of the literature and they ignored the commissioned independent advice group who deemed ACI to have a proven evidence base and to be economically viable. In fact, few of the treatments we use have a more solid evidence base and over 25 years in practice."
The following letter was submitted to NICE on behalf of BASK members, by Leela C Biant, BASK Representative Clinician Expert. The main points are:
- The consultation document produced by NICE has not taken into account all the relevant evidence,
- Has not appropriately interpreted the evidence,
- The provisional guidance is entirely unsound,
- The suggestions for further research are inappropriate and unethical.
The NICE Committee was provided with the UK Cartilage Consensus Paper, which is in press. It is due to be published in April 2015. It had 72 signatures of clinicians involved in cartilage repair in the UK (including Prof Vladimir Bobic) at the time it was submitted to NICE. It now has close to 100, which represents the majority of orthopaedic surgeons who perform this surgery. The Dutch Orthopaedic Society and the German Orthopaedic Society have previously published similar papers. One of the reasons the UK Cartilage Consensus Meeting was convened, was due to the previous NICE Appraisal being cited by NHS and other health providers to deny patients access to treatments where the clinicians consider the evidence to be strong enough to recommend ACI in appropriate patients.
Our response, which was communicated by email and at the BASK meeting was: "As we all know that has been going on for a long time and most NICE decisions about ACI were made with very limited input of people who are experienced specialists in cartilage repair. More importantly NICE has always insisted on clinical trials where ACI is often compared with microfracture or that ACI can be done only after failed microfracture. We know what happens when ACI is done after failed microfracture, from Tom Minas paper from 2009 on various problems like formation of intralesional osteoohytes, etc. So NICE is indirectly responsible for probably quite a few failed ACIs, because surgeons were advised to do microfracture first, or do ACI after microfracture fails. Insurance companies are using NICE NHS guidance as an excuse not to fund ACI surgery, and a few other "unproven" and "experimental" technologies so it is very likely that this situation is slow beginning of the end of ACI surgery in the UK."
Chondrocyte Therapy Effective in Knee Cartilage Repair
Medscape Medical News from the American Academy of Orthopaedic Surgeons (AAOS) 2015 Annual Meetin, Las Vegas. Laird Harrison, March 25, 2015:
Patients undergoing knee cartilage repair fare slightly better if the procedure includes autologous chondrocyte implantation, according to results from the ACTIVE trial. "At 5 years, we saw them moving ahead," said James Richardson, MD, from the Orthopaedic Hospital NHS Foundation Trust in Shropshire, United Kingdom. "This is a better cell than a stem cell," he told Medscape Medical News. "A chondrocyte is already determined to make cartilage." Previous clinical trials of chondrocyte implantation have shown some success, but Dr Richardson and his team wanted to test the procedure in a large randomized clinical trial that reflects the "real-world" variety of patients who might benefit from it.
The team recruited 390 patients from Norway and the United Kingdom who had previously undergone unsuccessful repair of the articular cartilage in their knees. "These are difficult patients," said Dr Richardson. Patients were randomly assigned to autologous chondrocyte implantation or to standard procedures, and an algorithm was used to ensure that the groups were balanced in number, age, size of defect, and preoperative Lysholm Knee Scoring Scale. The mean size of the defects was 3.2 cm, and 88% of them were on a femoral condyle; 64% of the patients were men. All the patients underwent surgery. The procedures, which varied depending on the recommendations of the surgeons, included debridement, abrasion, drilling, microfracture, mosaicplasty, and bone graft. Although patients improved on some measures of knee function, significant differences between the two groups did not emerge until year 5. By then, differences in Lysholm Knee Scoring Scale scores favored implantation (P = .11), as did differences in Cincinnati Knee Rating System scores, International Knee Documentation Committee scores (P = .02), EQ5D scores (P = .1), and satisfaction scores (P = .02).
Dr Richardson said he expects the differences to widen as cartilage continues to grow in the knees of the patients implanted with chondrocytes. The study is funded for another 5 years, he reported.
Interesting Linkedin Discussion: Does Cartilage Loss Cause Pain?
Does Cartilage Loss Cause Pain? We believe that pain comes from subchondral bone and synovium, not from chondral defects. But, altered architecture and biological (biomechanical) properties of diseased or injured articular cartilage trigger the process of subchondral remodelling (or degeneration) and reactive synovitis ... see the link above for further information.
Pinterest Arthroscopic and MR Image Boards
We are posting a selection of original arthroscopic and MR images from our daily clinical and surgical practice on Pinterest and Twitter. All images are anonymous and are intended to provide good quality visual information on typical knee problems but also normal knee anatomy for educational purposes. We will aim to Tweet a few selected images from time to time but all images will be available on Pinterest Arthroscopy and MRI boards. We are still thinking about posting some images on Instagram. Please let us know your thoughts (office@kneeclinic.info).
Please follow @ChesterKnee on Twitter for most recent articles, news and images
Other CKC News
Updated on 31 March 2015
Skiing: Zermatt, Switzerland, January 2015
We enjoyed a couple of days of skiing during the ICRS meeting, although the visibility was poor and the snow was less than perfect. "Proprioceptive" skiing (with very limited visual input) on icy slopes and in high winds was challenging but rewarding, with magnificent Matterhorn in the background, keeping an eye on us. Most importantly, we came back in one piece but with some very interesting GoPro footage (some of which which looks like a view from the inside of a tumble-dryer).

Skiing: Ortisei, Val Gardena and Sella Ronda, Italy, March 2015
Team CKC went to the Dolomites for a week to ski and explore this huge and well connected area. We were very lucky with fine sunny weather and generally good snow. We skied a lot and amongst many runs did the whole Sella Ronda and the Hidden Valley (8.5 km run from the top of the Lagazuoi to Armentarola).

We really liked South Tyrol (Alto Adige) as a region and in particular the area around Bolzano and Merano, which we also cycled in September 2014. A huge ski area is close to Bolzano and extends beyond the eastern side of South Tyrol.
This page was launched on 5 March 2014. Last update: 7 December 2015
Site last updated on: 28 March 2014
|
[ back to top ]

 Disclaimer: This website is a source of information
and education resource for health professionals and individuals
with knee problems. Neither Chester Knee Clinic nor Vladimir Bobic
make any warranties or guarantees that the information contained
herein is accurate or complete, and are not responsible for
any errors or omissions therein, or for the results obtained from
the use of such information. Users of this information are encouraged
to confirm the accuracy and applicability thereof with other sources.
Not all knee conditions and treatment modalities are described
on this website. The opinions and methods of diagnosis and treatment
change inevitably and rapidly as new information becomes available,
and therefore the information in this website does not necessarily
represent the most current thoughts or methods. The content of
this website is provided for information only and is not intended
to be used for diagnosis or treatment or as a substitute for consultation
with your own doctor or a specialist. Email
addresses supplied are provided for basic enquiries and should
not be used for urgent or emergency requests, treatment of any
knee injuries or conditions or to transmit confidential or medical
information. If you have sustained a knee injury or have a medical condition,
you should promptly seek appropriate medical advice from your local
doctor. Any opinions or information,
unless otherwise stated, are those of Vladimir Bobic, and in no
way claim to represent the views of any other medical professionals
or institutions, including Nuffield Health and Spire Hospitals. Chester
Knee Clinic will not be liable for any direct, indirect,
consequential, special, exemplary, or other damages, loss or injury
to persons which may occur by the user's reliance on any statements,
information or advice contained in this website. Chester Knee Clinic is
not responsible for the content of external websites.
Disclaimer: This website is a source of information
and education resource for health professionals and individuals
with knee problems. Neither Chester Knee Clinic nor Vladimir Bobic
make any warranties or guarantees that the information contained
herein is accurate or complete, and are not responsible for
any errors or omissions therein, or for the results obtained from
the use of such information. Users of this information are encouraged
to confirm the accuracy and applicability thereof with other sources.
Not all knee conditions and treatment modalities are described
on this website. The opinions and methods of diagnosis and treatment
change inevitably and rapidly as new information becomes available,
and therefore the information in this website does not necessarily
represent the most current thoughts or methods. The content of
this website is provided for information only and is not intended
to be used for diagnosis or treatment or as a substitute for consultation
with your own doctor or a specialist. Email
addresses supplied are provided for basic enquiries and should
not be used for urgent or emergency requests, treatment of any
knee injuries or conditions or to transmit confidential or medical
information. If you have sustained a knee injury or have a medical condition,
you should promptly seek appropriate medical advice from your local
doctor. Any opinions or information,
unless otherwise stated, are those of Vladimir Bobic, and in no
way claim to represent the views of any other medical professionals
or institutions, including Nuffield Health and Spire Hospitals. Chester
Knee Clinic will not be liable for any direct, indirect,
consequential, special, exemplary, or other damages, loss or injury
to persons which may occur by the user's reliance on any statements,
information or advice contained in this website. Chester Knee Clinic is
not responsible for the content of external websites.