Accelerated ACL Reconstruction Rehabilitation Program
About the Author: |
| Mark
De Carlo, PT, MHA, SCS, ATC, Chief Operating Officer Methodist
Sports Medicine Center, Indianapolis, Indiana, USA Mark has over 35 published articles and book chapters in the area of sports physical therapy. De Carlo received his Bachelor of Science degree in Secondary Education/Athletic Training from West Virginia University. He then received a Master of Science degree from the University of Indianapolis Krannert School of Physical Therapy. He is certified as a Sports Clinical Specialist by the American Board of Physical Therapy Specialties and has completed a Master of Science degree in Health Administration at Indiana University. Mark is currently serving as president of the Sports Physical Therapy Section of the American Physical Therapy Association, treasurer of the Journal of Orthopaedic and Sports Physical Therapy, Inc. Board of Directors and member-at-large of the International Federation of Sports Physiotherapy. |
This update on ACL rehabilitation was kindly written and put together
by Mark De Carlo and his team, exclusively for Chester Knee Clinic website,
for which we are very grateful. The text, images and videoclips should
not be used without author’s permission.
Rehabilitation following anterior cruciate ligament (ACL) reconstruction has changed dramatically over the past few decades. The staff of Methodist Sports Medicine Center in Indianapolis has over 15 years experience with patients sustaining injury to the anterior cruciate ligament. Over this time we have developed a progressive philosophical approach to rehabilitation following ACL reconstruction.
Our present philosophy on rehabilitation following ACL reconstruction has evolved through observation of our patients and documented clinical results. We have continually attempted to modify and update our protocol as a means of improving patients’ final outcome following surgical reconstruction. The ideal situation is one in which the patient with ACL deficiency undergoing surgical reconstruction will ultimately have a result of excellent stability, full range of motion and strength, and normal function.
Conventional rehabilitation emphasized early protection of the ACL reconstructed knee by restricting knee motion, weight bearing, and rate of return to functional activities. In 1982, the surgical leg was placed in a cast at 30 degrees of flexion to avoid excessive graft stress. Weight bearing without a brace was not allowed for 6-8 weeks following surgery and most patients were restricted from full participation in sports activities for the first year. The high rate of postoperative complications, including permanent knee stiffness, knee pain and low predictability with return to high level sports, has brought about a number of changes in ACL postoperative rehabilitation.
In 1985, we conducted a study comparing compliant patients with those
who progressed more rapidly than we recommended (noncompliant patients).
To our surprise, the noncompliant patients demonstrated fewer long-term
knee motion problems and fewer subjective complaints than their compliant
counterparts, without difference in long-term stability. Through this
process, we learned that:
-
an early loss of knee extension often led to long-term loss of extension accompanied by subjective symptoms,
-
patients who failed to regain early leg control often struggled with regaining full quadriceps muscle strength later on, and
-
patients who returned to sporting activities before recommended had similar knee stability to patients who were compliant with our restrictions.
This helped us to place emphasis on factors felt to be of primary importance. These include:
- restoration of full hyperextension equal to the uninvolved knee,
- regaining of good quadriceps muscle leg control, and
- allowing for early wound healing.
Phase I (Preoperative)
Rehabilitation for the injured knee begins immediately following ACL injury. The clinical goals for Phase I include restoring full range of motion (ROM) and normal strength and control swelling prior to surgery. Patients are also to completely understand the basic principles of accelerated rehabilitation including full terminal knee extension, early weight bearing, and closed and open chain strengthening. The time needed to accomplish these goals can be as little as 1 week or as long as 2 months, depending on how the knee responds to the initial injury.
To reduce swelling, a cold compression cuff (Cryo/Cuff) (Fig. 1) is applied to the knee and filled with ice-cold water. The patient can wear the cuff continually except when walking. Swelling reduction eases the return of normal range of motion.
 |
Returning full knee range of motion equal to the uninvolved knee prior to surgery decreases complications such as post-operative knee stiffness. To restore full range of motion, the patient is instructed in several exercises including heel props (Fig. 2), prone hangs (Fig. 3), and towel extensions (Video 1) for extension and wall slides (Video 2) and heel slides (Video 3) for flexion. If the patient has problems attaining full terminal extension with the exercises, he or she may be giving a hyperextension device (extension board) (Fig. 4) to assist in gaining full hyperextension. |
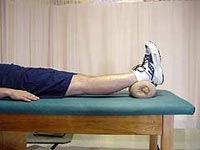
Figure 2 |

Figure 3 |

Figure 4 |
Encouraging the patient to move from partial to full weight bearing as tolerated stresses the importance of restoring a normal gait. Full passive extension and quadriceps control is necessary before normal gait con be accomplished. Therefore, the emphasis of gait instruction is on achieving full knee extension at heel strike with full weight bearing on the involved side. The patient is expected to be walking normally prior to surgery.
To encourage early strengthening, the patient is instructed in several closed kinetic chain exercises including leg press (Fig. 5), squats (Fig. 6), step-downs (Fig. 7), bike (Fig. 8), and Stairmaster (Fig. 9). These exercises are introduced after swelling from the injury has decreased and ROM has been restored.

Figure 5 |

Figure 6 |

Figure 7 |

Figure 8 |

Figure 9 |
During the initial evaluation, the functional demands of the patient are assessed including activities of daily living and athletic and recreational activities. School, work, and family schedules are also examined to determine the most appropriate time to schedule surgery.
Phase I also includes patient counseling on the concepts of our approach to rehabilitation, the timing of surgery with details of the reconstructive procedure, and specific postoperative rehabilitation goals and expectations. Because mental preparation is a very important aspect of success of the surgical reconstruction and rehabilitation, it is essential that the patient understand the goals of rehabilitation process and how these goals will be achieved.
Phase II (Immediate Postoperative)
The clinical goals of Phase II include decreasing swelling, obtaining full passive knee extension, and obtaining 110 degrees of flexion. Additional variables include performing an independent straight leg raise and restoring normal walk.
Phase IIa: (1 to 6 days)
To minimize pain and swelling, a Cryo/Cuff is placed on the patient’s knee immediately following the operation. The Cryo/Cuff remains on the knee at all times, except when performing motion exercises. Continuous passive motion is initiated following discharge from the recovery room and the machine is set to 0-30 degrees. The CPM machine is to remain on, with the patient’s leg in it at all times, except when doing motion exercises and going to the bathroom.
Exercises for regaining full ROM are begun the day of surgery. Hyperextension is maintained with 10 minutes of heel prop exercises every waking hour. Flexion exercises are performed six times daily. This can easily done by slowly increasing flexion of the CPM machine to the 110 degrees and holding the position for 10 minutes four times a day. Once maximal flexion has been attained in the CPM machine, patients can continue to increase bend beyond 110 degrees by pulling leg further to buttocks with their hands.

Figure 10 |
Leg-control exercise is started on the day of surgery and consists of quadriceps contraction exercises and independent straight leg raises. Active heel height exercises (Figure 10) are performed to promote leg control and to minimize the potential for a patellar contracture. During the first week patients are to remain lying down as much as possible. However, when getting up to go to the bathroom patients is encouraged to be weight bearing as tolerated. Crutches may be used for the first few days to facilitate a normal walking pattern
The patient will report to physical therapy one week after surgery and should have full terminal extension and flexion to 110 degrees, minimal swelling and soft tissue healing, and normal walking.
Phase IIb: (7 to 14 Days)
The patient is evaluated at the one-week visit by both the surgeon and the physical therapist. The patient’s rehabilitation program is advanced concentrating on swelling control, ROM, quadriceps leg control, and walking.
Regaining full extension range of motion is the most critical factor in this phase. Full hyperextension is maintained with heel prop and prone hang exercises. As in the preoperative phase, if the patient has problems maintaining full hyperextension, an extension board may be used. The CPM is discontinued at one week. Flexion range of motion is progressed with wall slides and heel slides. The Cryo/Cuff is stilled used on a regular basis to control swelling when the patient is not performing exercises.
The patient is encouraged to progress from partial to full weight bearing without crutches (Video 4). Walking activities involve heel to toe walking, retro-walking, and high-knee activities. The focus on retro-walking is to fully extend the knee when going from toe to heel. Practicing walking in front of a mirror greatly aids in the return of a normal walking pattern. The mirror gives patients an immediate visual cue as to how they are walking. It is very important to emphasize leg control early in the rehabilitation program. Through early extension and normal gait the patient is able to regain good quadriceps tone and leg control. This combination of clinical variables will set the pace for the entire rehabilitation program and a successful outcome.
The patient is encouraged to lock out the knee by standing with the weight shifted to the ACL reconstructed leg so that extension is full and the knee is fully locked (Video 5). This exercise is referred to as single leg stance and is preferred whenever the patient is standing. Single leg stance on the involved leg is an effective method of working on full ROM and leg control, while giving the patient confidence in standing on the injured leg to begin to do functional activities.
Once the patient has regained full knee extension and is ambulating normally it is possible to implement strengthening exercises. Leg strengthening exercises include bilateral one-quarter knee bends and calf raises. It is felt that this type of exercise facilitates return of lower extremity strength with minimal stress to the joint.
Patients will return 2 weeks following surgery for a physician and therapy visit. At that time, the patient should have full extension, flexion to 130 degrees, controlled swelling, normal walking, and able to return to school or sedentary work.
Phase III: (2 to 4 weeks)
Phase III begins at the second postoperative visit two weeks after surgery. Clinical goals for Phase III include full terminal extension and full flexion to 130 degrees, consistent weight room and moderate speed strengthening, and early return to agility and sports specific drills.
Maintaining full knee extension is continued with exercises including prone hangs, passive and active heel lift, and, if needed, a hyperextension device. Increasing flexion is achieved by exercises such as heel slides and by using a stationary bike to facilitate flexion ROM.
Functional strengthening is initiated once the patient has sufficient leg control to perform a unilateral knee bend without difficulty. Exercises include one-quarter squats, unilateral leg press, unilateral calf raises, unilateral step-downs, Stairmaster, and riding the stationary bike. Swimming and other hydrotherapy exercises can be started once the incisions have healed. Our preferred exercise progression includes short arc quadriceps from 90 to 30 degrees, knee bends, step-ups and leg press. These exercises are started with lower weight and then gradually progressed to higher weight with lower repetitions.
If full ROM and other goals have been met sport specific and agility drills may be initiated including jump rope, single leg hop, and easy position drills.
After Phase III, the patient will return to physical therapy every 4 to 6 weeks until 6 months, then again at 9, 12, and 24 months following surgery.
Phase IV: (4 weeks on)
The emphasis in Phase IV is on advanced strengthening and return to sports. To advance into the final phase of the rehabilitation program, the patient needs to have nearly full ROM. Our goal is to reach this phase by four to five weeks after surgery. However, if the patient has not achieved the goals of the previous phase, advanced agility and sport specific activities are not yet initiated. The clinical goals for Phase IV include full ROM including terminal extension, improved quadriceps tone, at least 70% strength, agility specific program, complete a sport specific functional progression and return to full activity.
Exercise instruction includes an increase in weight room and home strengthening activities. Exercises include unilateral leg press, unilateral leg extensions, unilateral step-downs, unilateral calf raises, full squat to no more than 90 degrees, and lunges. Patients are encouraged to progress from high repetition/low weights to low repetition/high weights. Also, some type of moderate speed strength and cardiovascular activity should be continued such as bicycling, swimming, or using a Stairmaster.
The patient’s first visit during Phase IV is four weeks after surgery. This visit will include the first isokinetic strength test (Fig. 11), a isometric leg press test (Fig. 12) and a KT-1000 ligamentous stability test (Fig. 13).

Figure 11 |

Figure 12 |

Figure 13 |
Factors influencing the patient’s return to controlled agility training and sport specific activity includes the patient subjective rating, as well as isokinetic and isometric test scores. If the patient’s strength ratio is at least 65%, agility activities are started. These activities include lateral shuffles, cariocas, cross over drills, and backward running. Patients may also begin solo sports such as shooting a basketball or hitting a racquetball. These early agility activities promote patient confidence, facilitate moderate-speed strength, and re-develop quickness, agility, and sport specific skills. As the patient progresses, agility workouts become more vigorous to include activities such as figure of eights and half to full speed running. The speed of progression is based on the specific athletic and recreational desires of the patient. Sports specific activities are incorporated into the progression with specific focus on athletic goals.
Although many patients ask “when can I start running again” at the beginning of Phase IV, running for conditioning or rehabilitation actually is the final step in the rehabilitation process. We prefer that the patient work on agility drills and sport specific skills instead of running two to three miles. Running long distances at this time leads to swelling and, therefore, can cause a delay in the rehabilitation process.
The athlete must participate in sport specific activities. Although we allow them to and they can successfully return to practice and playing early after surgery, it can take two to three months of sport specific activities (both practicing and playing) before the athlete will feel completely comfortable with their knee and recover 100% of their quickness.
The patient is followed every four to six weeks for up to six months, but is allowed to return to practice and playing as they feel comfortable and as our evaluation allows. Specific testing strategies at each visit consist of isokinetic and isometric strength testing, single leg hop, and KT-1000 measurements.
Site last updated on: 28 March 2014
|
[ back to top ]





 Disclaimer: This website is a source of information
and education resource for health professionals and individuals
with knee problems. Neither Chester Knee Clinic nor Vladimir Bobic
make any warranties or guarantees that the information contained
herein is accurate or complete, and are not responsible for
any errors or omissions therein, or for the results obtained from
the use of such information. Users of this information are encouraged
to confirm the accuracy and applicability thereof with other sources.
Not all knee conditions and treatment modalities are described
on this website. The opinions and methods of diagnosis and treatment
change inevitably and rapidly as new information becomes available,
and therefore the information in this website does not necessarily
represent the most current thoughts or methods. The content of
this website is provided for information only and is not intended
to be used for diagnosis or treatment or as a substitute for consultation
with your own doctor or a specialist. Email
addresses supplied are provided for basic enquiries and should
not be used for urgent or emergency requests, treatment of any
knee injuries or conditions or to transmit confidential or medical
information. If you have sustained a knee injury or have a medical condition,
you should promptly seek appropriate medical advice from your local
doctor. Any opinions or information,
unless otherwise stated, are those of Vladimir Bobic, and in no
way claim to represent the views of any other medical professionals
or institutions, including Nuffield Health and Spire Hospitals. Chester
Knee Clinic will not be liable for any direct, indirect,
consequential, special, exemplary, or other damages, loss or injury
to persons which may occur by the user's reliance on any statements,
information or advice contained in this website. Chester Knee Clinic is
not responsible for the content of external websites.
Disclaimer: This website is a source of information
and education resource for health professionals and individuals
with knee problems. Neither Chester Knee Clinic nor Vladimir Bobic
make any warranties or guarantees that the information contained
herein is accurate or complete, and are not responsible for
any errors or omissions therein, or for the results obtained from
the use of such information. Users of this information are encouraged
to confirm the accuracy and applicability thereof with other sources.
Not all knee conditions and treatment modalities are described
on this website. The opinions and methods of diagnosis and treatment
change inevitably and rapidly as new information becomes available,
and therefore the information in this website does not necessarily
represent the most current thoughts or methods. The content of
this website is provided for information only and is not intended
to be used for diagnosis or treatment or as a substitute for consultation
with your own doctor or a specialist. Email
addresses supplied are provided for basic enquiries and should
not be used for urgent or emergency requests, treatment of any
knee injuries or conditions or to transmit confidential or medical
information. If you have sustained a knee injury or have a medical condition,
you should promptly seek appropriate medical advice from your local
doctor. Any opinions or information,
unless otherwise stated, are those of Vladimir Bobic, and in no
way claim to represent the views of any other medical professionals
or institutions, including Nuffield Health and Spire Hospitals. Chester
Knee Clinic will not be liable for any direct, indirect,
consequential, special, exemplary, or other damages, loss or injury
to persons which may occur by the user's reliance on any statements,
information or advice contained in this website. Chester Knee Clinic is
not responsible for the content of external websites.